Category Archives: Jacksonville
Entry into the Leading Physicians of the World
Life-saving treatments learned from war being missed
 Trauma is responsible for more global deaths annually than HIV, malaria and tuberculosis combined. Yet healthcare systems in many countries are missing out on life-saving treatments learned on the battlefield, according to a review by King’s College London and published today in the Journal of the Royal Society of Medicine.Medical advancements made by the military in times of conflict, are increasingly seen in the hospitals of high income countries but are being missed in poorer countries, where trauma is the leading cause of death in young people. Many innovations by frontline doctors in stabilising and treating severely wounded soldiers could be adapted for use in other healthcare settings.The review was conducted by the Centre for Global Health at King’s College London, in collaboration with the International Prevention Research Institute (IPRI). It calls for research and changes in policy to determine how innovations in military medicine can be transferred to civilian populations, particularly in low-resource regions where the more simple and cost-effective of these medical advances could be implemented.
Trauma is responsible for more global deaths annually than HIV, malaria and tuberculosis combined. Yet healthcare systems in many countries are missing out on life-saving treatments learned on the battlefield, according to a review by King’s College London and published today in the Journal of the Royal Society of Medicine.Medical advancements made by the military in times of conflict, are increasingly seen in the hospitals of high income countries but are being missed in poorer countries, where trauma is the leading cause of death in young people. Many innovations by frontline doctors in stabilising and treating severely wounded soldiers could be adapted for use in other healthcare settings.The review was conducted by the Centre for Global Health at King’s College London, in collaboration with the International Prevention Research Institute (IPRI). It calls for research and changes in policy to determine how innovations in military medicine can be transferred to civilian populations, particularly in low-resource regions where the more simple and cost-effective of these medical advances could be implemented.
Read the rest of the article at http://www.medicalnewstoday.com/releases/291231.php.
Newly identified compounds in spider venom could help treat chronic pain
 The thought of spiders may make your skin crawl, but a new study suggests that maybe we should put our hatred of the eight-legged beasts to one side; their venom could lead to a more effective treatment for the 100 million Americans who suffer from chronic pain.Chronic pain – defined as pain that lasts longer than 3-6 months – is the most common cause of long-term disability in the US. It occurs when nerves in a part of the body send continuous signals to the brain via pain pathways.Past studies have found that, in humans, one of the most common pathways involved in chronic pain is Nav1.7. The researchers of this latest study – led by Prof. Glenn King of the Institute for Molecular Bioscience at The University of Queensland in Australia – believe targeting this pathway could help treat a wide range of pain conditions.”A compound that blocks Nav1.7 channels is of particular interest for us,” says Prof. King. “Previous research shows indifference to pain among people who lack Nav1.7 channels due to a naturally-occurring genetic mutation – so blocking these channels has the potential of turning off pain in people with normal pain pathways.”
The thought of spiders may make your skin crawl, but a new study suggests that maybe we should put our hatred of the eight-legged beasts to one side; their venom could lead to a more effective treatment for the 100 million Americans who suffer from chronic pain.Chronic pain – defined as pain that lasts longer than 3-6 months – is the most common cause of long-term disability in the US. It occurs when nerves in a part of the body send continuous signals to the brain via pain pathways.Past studies have found that, in humans, one of the most common pathways involved in chronic pain is Nav1.7. The researchers of this latest study – led by Prof. Glenn King of the Institute for Molecular Bioscience at The University of Queensland in Australia – believe targeting this pathway could help treat a wide range of pain conditions.”A compound that blocks Nav1.7 channels is of particular interest for us,” says Prof. King. “Previous research shows indifference to pain among people who lack Nav1.7 channels due to a naturally-occurring genetic mutation – so blocking these channels has the potential of turning off pain in people with normal pain pathways.”NSAIDS linked to risk of bleeding in heart attack patients
 Even short-term treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen increases the risk of bleeding in patients taking anti-clotting drugs after a heart attack, a study published in JAMA suggests.All patients who have had a myocardial infarction (MI) are recommended to take two antithrombotic drugs (aspirin and clopidogrel) as preventive treatment for up to a year after the heart attack, and to continue taking one of the anti-clotting pills thereafter.Risk of bleeding is known to be increased by then adding the use of NSAIDs, and some – ibuprofen, for example – have a counter effect to the preventive heart drugs, inhibiting the antithrombotic effects of aspirin.Guidelines from the American Heart Association, therefore, recommend against the use of NSAIDs in people with established heart disease.
Even short-term treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen increases the risk of bleeding in patients taking anti-clotting drugs after a heart attack, a study published in JAMA suggests.All patients who have had a myocardial infarction (MI) are recommended to take two antithrombotic drugs (aspirin and clopidogrel) as preventive treatment for up to a year after the heart attack, and to continue taking one of the anti-clotting pills thereafter.Risk of bleeding is known to be increased by then adding the use of NSAIDs, and some – ibuprofen, for example – have a counter effect to the preventive heart drugs, inhibiting the antithrombotic effects of aspirin.Guidelines from the American Heart Association, therefore, recommend against the use of NSAIDs in people with established heart disease.Distraction techniques may reduce pain, anxiety during conscious surgery
 For some surgical procedures – such as the removal of varicose veins – the patient remains awake. Though safe, the patient can experience some pain and anxiety. But in a new study, researchers from the University of Surrey in the UK say simple methods of distraction could help ease such experiences.
For some surgical procedures – such as the removal of varicose veins – the patient remains awake. Though safe, the patient can experience some pain and anxiety. But in a new study, researchers from the University of Surrey in the UK say simple methods of distraction could help ease such experiences.
To reach their findings, published in the European Journal of Pain, Prof. Jane Ogden and colleagues enrolled 398 patients who were due to undergo varicose veinsurgery.For this type of surgery, patients typically remain awake, receiving only a local anesthetic.The researchers note that previously, patients have reported unfamiliar feelings, sounds and smells during the procedure. Some have also reported feeling a burning sensation, while others have said listening to conversations about the procedure between the surgeon and nurse makes them feel uneasy. Patients have also reported feeling anxious during the surgery.
Read the rest of the article at http://www.medicalnewstoday.com/articles/288755.php
The Royal College of Anaesthetists calls for joined up care for high risk surgical patients
The Royal College of Anaesthetists (RCoA) shared its vision for the future of perioperative healthcare provision across the UK. Speaking at a stakeholder event, President of the RCoA Dr J-P van Besouw said: “With more than ten million patients undergoing surgery each year in the NHS, approximately 15% of whom are deemed to be high-risk, a care pathway that can harness multi-disciplinary working, reduce variation and improve patient outcomes must be our goal.”
Health experts, including Celia Ingham Clark, Director for Reducing Premature Mortality, NHS England, highlighted the scale of the unmet need for the high-risk surgical patient and the future principles for a more efficient and effective care pathway, at the event attended by a cross section of health bodies.
J-P van Besouw said: “Lowering the rate of avoidable harm – associated with many preventable complications and deaths – will make a significant saving to the NHS annual surgical bill, which at present runs at around GBP16 billion. The College believes that improved perioperative care is an efficient and effective solution.”
The RCoA proposed that care pathways designed around the individual needs of the complex surgical patient and delivered by a multi-disciplinary perioperative care team would mean that patients should receive the most appropriate care possible. Anaesthetists are uniquely positioned to lead such teams and to ensure a better continuum of care for patients, before, during and after surgery. Such an integrated approach should minimise inappropriate care, reduce cancellations, complications and readmissions and ensure quicker recovery and discharge from hospital. Fundamentally patients should receive better quality care, and experience better outcomes at a lower cost.
As well as improved patient centered care, the economic case for change is an important factor to be considered. The NHS Five Year Forward view states that by 2020/21, there could be a mismatch between resources and patient needs of nearly GBP30 billion a year. Demand, efficiency and funding are the key considerations and the evidence would indicate that perioperative medicine would be a cost effective solution through the reduced costs of treating complications.
In driving this agenda the College stated that it intended to work collaboratively with stakeholders in primary care, other colleges, specialties and workforce planners in Health Education England (HEE) and the devolved nations, to develop and commission new standards of patient care, embed continuous data driven quality improvement into the care of surgical patients, and explore solutions to create an appropriate workforce for a sustainable future.
“We do not underestimate the challenges that we face in delivering this agenda,” said J-P van Besouw. “We are asking colleagues, policy makers and commissioners to share this vision and to use the resources that we have developed, including a short animated film [http://www.rcoa.ac.uk/periopmed/animation], to start the conversation on what perioperative practice should look like and to work with us to develop integrated pathways of care, based on the many existing examples of excellent perioperative practice from across the UK.”
Adapted by MNT from original media release
http://www.medicalnewstoday.com/releases/288455.php
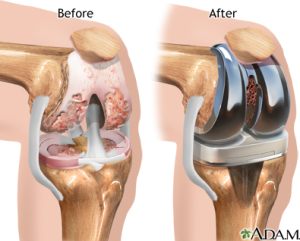
An alternative for pain control after knee replacement surgery
It’s estimated that more than half of adults in the United States diagnosed with knee osteoarthritis will undergo knee replacement surgery. While improvements in implantable devices and surgical technique has made the procedure highly effective, pain control after surgery remains a common but persistent side effect for patients.
A Henry Ford Hospital study, presented recently at the American Association of Hip and Knee Surgeons meeting in Dallas, found that injecting a newer long-acting numbing medicine called liposomal bupivacaine into the tissue surrounding the knee during surgery may provide a faster recovery and higher patient satisfaction.
“The pain scores for this injection technique averaged about 3/10, which is similar to the pain scores seen with our traditional method,” says Jason Davis, M.D., a Henry Ford West Bloomfield Hospital joint replacement surgeon and the study’s senior author. “Patients had pain relief for up to two days after surgery and better knee function compared with the traditional method.”
It is estimated that the number of total knee replacement surgeries has more than tripled from 1993 to 2009. Arthritisis the most common cause of chronic knee pain and disability. However, a June 2014 study found that 95 percent of knee surgeries are attributed to the epidemic of overweight and obesity in the United States.
During the two-hour knee replacement procedure, the orthopedic surgeon removes the damaged cartilage and bone, and inserts a knee implant to restore the alignment and function of the knee. More than 90 percent of knee replacements are functioning 15 years after surgery, according to the American Academy of Orthopaedic Surgeons.
In the Henry Ford study, 216 patients were evaluated for pain control the first two days after surgery from October 2012 to September 2013. Half of the patients received the traditional pain control method with continuous femoral nerve blockade, in which common numbing medicine is injected into the groin area, blunting the main nerve down the front of the knee. This method uses a pain pump to extend pain control for two days but causes some leg weakness. “Pain control came at the price of weakness and made patients somewhat tentative when walking during their hospital stay,” Dr. Davis says.
The other half of patients received the liposomal bupivacaine injection at the site of the surgery.
Dr. Davis says many patients were able to walk comfortably within hours after surgery.
Dr. Davis says the injection around the knee itself “optimizes pain control early on” without the side effects of the traditional technique. “Function-wise, it was a lot easier for patients to move around more confidently,” he says. “In the past decade, we’ve made major advancements in pain control for knee replacement surgery. This option is a promising, viable one for our patients.”
Adapted by MNT from original media release
http://www.medicalnewstoday.com/releases/287423.php
The difficulties of treating shoulder pain in baseball pitchers
Results of treating shoulder pain in baseball pitchers and other throwing athletes are not as predictable as doctors, patients and coaches would like to think, according to a report in the journal Physical Medicine and Rehabilitation Clinics of North America.
Nickolas Garbis, MD, an orthopedic surgeon who specializes in shoulder and elbow injuries at Loyola University Medical Center, is the primary author.
Shoulder pain occurs in athletes who play sports that require rapid acceleration and deceleration of the throwing arm. They include baseball pitchers, tennis players, softball pitchers and javelin throwers, as well as athletes who play handball and water polo.
Overhead throwing generates a large amount of stress on the shoulder, which is one of the most mobile joints in the body. This makes it vulnerable to injury.
It is difficult to diagnose the cause of shoulder pain. The shoulder is comprised of four joints, and a problem with any of them can cause pain and affect performance. Moreover, many of these structures are deep in the shoulder and therefore difficult to examine by touch. Also, the same kind of pain can be due to multiple causes. For example, pain in the front of the shoulder can be due to rotator cuff tendinitis, rotator cuff tears, biceps tendinitis, shoulder instability, shoulder stiffness and several other causes.
“A systemic approach, and some experience, can help the clinician become more familiar with which constellation of findings in these athletes is not normal,” Dr. Garbis and co-author Edward McFarland, MD, write.
Shoulder problems can begin during adolescence. Little League shoulder, an injury to the growth plate in the shoulder, is one of the most common. Adolescent pitchers most at risk for injuries are those who compete on traveling teams. Overuse injuries can lead to more serious mechanical injuries. Adhering to pitch counts should reduce injuries and decrease fatigue.
Treatment should be primarily nonsurgical. Nonsurgical options include icing the shoulder and judicial use of nonsteroidal anti-inflammatory medications such as ibuprofen and naproxen. Rehabilitation can restore a normal muscular balance. Rest can help, but it should not be prolonged, because the shoulder could become deconditioned.
If nonsurgical options fail, arthroscopic surgery can be considered. For example, surgical repair or trimming of partial rotator cuff tears can be highly successful, returning as many as 89 percent of college and professional pitchers back to play. However, the type of surgery needed depends upon the patient’s shoulder problem.
http://www.medicalnewstoday.com/releases/286793.php
Pain relief for kids in the ER without a needle
Children in emergency departments can safely be treated for pain from limb injuries using intranasal ketamine, a drug more typically used for sedation, according to the results of the first randomized, controlled trial comparing intranasal analgesics in children in the emergency department. The study was published online recently in Annals of Emergency Medicine (“The PICHFORK (Pain in Children Fentanyl OR Ketamine) Trial: A Randomized Controlled Trial Comparing Intranasal Ketamine and Fentanyl for the Relief of Moderate to Severe Pain in Children with Limb Injuries”).
“This is great news for emergency physicians and their young patients, especially those who may not tolerate other intranasal pain medications such as fentanyl,” said lead study author Professor Andis Graudins, MD, of Monash University in Clayton, Victoria, Australia. “For children in pain and distress, the option of treating their pain without a needle is a huge benefit as well. The intranasal option using fentanyl is accepted already for children, but the safe use of ketamine is new.”
Researchers compared pain relief resulting from ketamine and fentanyl, both delivered intranasally, for children 3 to 13 years old whose pain from isolated limb injuries registered seven or higher on a 10 point scale. Median baseline pain rating was eight out of ten. After 30 minutes, the median reductions in pain for ketamine were 4.45 and for fentanyl were 4.0. The pain reduction was maintained in both groups at 60 minutes. Satisfaction for ketamine was slightly higher at 83 percent. Fentanyl had a 72 percent satisfaction rating.
Adverse events were reported more frequently for ketamine (78 percent of patient) than for fentanyl (40 percent of patients), but they were all mild (dizziness or drowsiness were common).
“Ketamine is a great alternative for injured children in the ER who may not be able to tolerate opiates, like fentanyl,” said Prof. Graudins. “And being able to deliver pain-relief with minimal upset, such as that triggered in some children by even the sight of needles, is a great boon to our youngest patients.”
http://www.medicalnewstoday.com/releases/286526.php